Osteochondrosis -degenerative-dystrophic damage to the tissues of the spine, characterized by damage to the intervertebral discs, adjacent joint surfaces, and vertebral bodies, the spinal cord device.
Most often, the pathological processes of osteochondrosis first affect the bones and ligaments. The fact that the disease has already begun is usually learned when complications appear - pain, sensory disturbances, muscle atrophy, disruption of internal organs.
Who suffers from osteochondrosis?
Today, 40-90% of the world’s population suffers from osteochondrosis. Most often, the disease affects people over 30 years of age. However, the first symptoms of osteochondrosis can occur in adolescence.
Developmental stages of spinal osteochondrosis
- The first stage in the development of osteochondrosis.
Dehydration of the pulpos nucleus begins. This leads to a decrease in the height of the plate. Cracks appear in the annulus fibrosus, but the pathological process does not extend beyond the intervertebral disc.
- The second stage in the development of osteochondrosis.
As the height of the disc decreases, the points of attachment of the muscles and ligaments belonging to the two adjacent vertebrae get closer. Therefore, the muscles and ligaments sag. This can lead to excessive mobility of the two vertebrae relative to each other, i. e. instability of the vertebral motor segment develops. This stage is characterized by the relative displacement or displacement of the vertebrae with the development of spondylolisthesis.
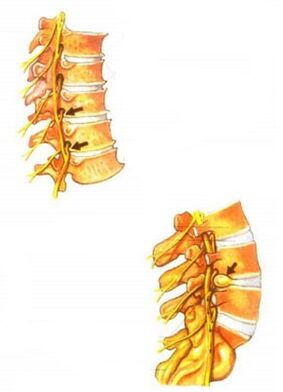
- The third stage in the development of osteochondrosis.
It is during this period that the most pronounced morphological changes occur, which primarily affect the intervertebral discs themselves: prolapses and protrusions of the plates occur. The vertebral device of the vertebral motor segment also suffers. Subluxations occur in the intervertebral joints and unco-vertebral joints, arthrosis is formed.
- The fourth stage in the development of osteochondrosis.
At this stage, adaptive changes occur in the affected segments of the spine. The body tries to overcome the excessive mobility of the vertebrae, immobilizing the spine to maintain its supportive and protective functions. In this regard, marginal bone growths appear on adjacent surfaces of vertebral bodies, in other words, osteophytes. An osteophyte grown in the "wrong place" causes microtraumatization of the nerve root. In the fourth stage, the processes of fibrous ankylosis usually begin in the intervertebral discs and joints. Finally, it turns out that the vertebral motor segment seems to be masonry in a shell - clinical manifestations subside.
Causes of osteochondrosis
Each of the many existing theories of the development of osteochondrosis accepts different causes that are responsible for the development of the disease, such as mechanical injuries, hereditary predisposition, or metabolic disorders. A particular difficulty in determining the cause of osteochondrosis is the fact that this disease can occur in both the elderly and the young, both physically fit and less educated. It is widely believed that the cause of osteochondrosis is the deposition of salts in the spine: X-rays are said to show salt in the form of "outgrowths" or "hooks" on the vertebrae. If cracks and crackles are seen in the joints as they move, as if sand is being poured between them, the only cause of this condition for many patients is the infamous "salt deposit. "Such misconceptions are not harmless at all: the correct idea of how to treat the disease can be determined on the basis of an analysis of the causes.
The term "osteochondrosis" is derived from the Greek roots of osteon - "bone" and chondr - "cartilage". The suffix "-oz" means that the disease of the bone and cartilage is not associated with inflammatory processes, it is degenerative-dystrophic in nature, i. e. the disease is based on tissue malnutrition and consequently tissue degeneration. structure. Like all living tissues, the bone tissue of the vertebrae and the cartilage tissue of the intervertebral disc are constantly rearranged and self-renewed. As a result of regular physical exertion, they gain strength and flexibility, and in the absence of loads, the strength of the tissues decreases.
This is due to the specifics of nutrition and the blood supply to the bone and cartilage tissues. Adult discs have no blood vessels of their own, receiving nutrients and oxygen from adjacent tissues. Therefore, for proper nutrition of the plates, blood circulation in the tissues surrounding the discs must be activated. And this can only be achieved with intense muscular work.
According to its composition, the intervertebral disc can be divided into two parts: this gelatin core, which gives the disc flexibility, is located in the middle, and the strong fibrous ring surrounding it. Due to the deterioration of the nutrition of the intervertebral plates, the complex structure of the biopolymer compounds that make up the nucleus pulposus is destroyed. The moisture content of the gelatinous seed decreases and becomes more brittle. Even when exposed to minor overloads, the gelatinous core can disintegrate. This leads to an even greater decrease in flexibility. The strength of the fibrous disk rings also decreases. All of these factors underlie the cause of osteochondrosis.
Restoration of the function of the spine requires scarring of the intervertebral disc, mobilization of the compensatory abilities of the spine and the entire musculoskeletal system, and not resorption of the "salt deposits". elimination of "thorns" on the vertebrae. X-ray examination after the end of the treatment shows that the vertebrae did not change their shape. And the infamous "thorn" is not the cause of osteochondrosis, but a consequence of adaptive processes. Marginal increases increase the area of the vertebral body support surface. As the area increases, the specific pressure decreases, allowing the strength and flexibility of the intervertebral disc to decrease.
Degenerative-dystrophic changes in the spine are associated with calcification (calcification) of damaged sections, articular ligaments, cartilage, and certain sections of capsules. This process can only be called salt deposition. Thus, this is not the cause of osteochondrosis, but only a consequence and final stage of the above process.
Reverse development of spinal structural changes is almost impossible. But keeping it as low as possible is a very real challenge. If we do not try to keep the spine in the state we have achieved with the treatment, the pain may recur.
Clinical manifestations of osteochondrosis
The clinical manifestations of osteochondrosis are very diverse. They depend on the stage of development of osteochondrosis. The main clinical symptoms of osteochondrosis occur when the pathological process extends to the posterior part of the annular fibrosis and the posterior longitudinal ligament. Depending on the stage of degeneration of the intervertebral discs, irritation, compression or decreased conductivity of the roots of the spinal cord, vascular or spinal cord compression occurs. Different neurological syndromes develop - reflex and compression.
The main cause of pain in osteochondrosis is called nerve root irritation. In this case, circulatory disorders occur, edema occurs, and in the future fibrosis of the surrounding structures may develop, which is accompanied by an increase in the sensitivity of the roots to various effects (movements in the affected segment of the spine, etc. ).
In osteochondrosis, vascular disorders are often associated with damage to vasomotor innervation. Mechanical compression of blood vessels by osteophytes, such as in the cervical spine, is also possible.
Symptoms of osteochondrosis
One of the characteristics of osteochondrosis of the spine, which aggravates the process, is the symptoms that are too extensive. The disease can manifest in completely different parts of the body. There may be pain or numbness in the limbs, or abnormalities and pain in the internal organs. However, often a person does not in any way associate pain in the heart region, genital dysfunction, headache, pain and numbness in the legs in osteochondrosis and in the spine in general, direct "treatment" of osteochondrosis symptoms with various painkillers, all kinds of advertised medicationsusing accessories and other methods. But this path only exacerbates the situation. Osteochondrosis continues to develop, and the treatments used simply do not lead to significant improvement at best, except for temporary pain relief, and at worst can further damage the body.
Therefore, it is important to thoroughly analyze its condition and the changes taking place in it. You need to start moving in the right direction: see a doctor in time, perform the necessary diagnostics, and only start treatment under the supervision of your doctor once the correct diagnosis has been made.
The main symptoms of osteochondrosis are mainly back pain and discomfort. However, the pains can be periodic, unstable in nature, now appearing and then disappearing. But even the first discomfort or pain in the spine makes you think. The appearance of the first pains is an indication that we should at least pay attention to it, try to remember the reason why they appeared. This can be caused by lifting a heavy object, sudden movement, falling, etc.
Another symptom of osteochondrosis is accompanied by discomfort or back pain with pain and numbness in the limbs (arms or legs). The pain most often radiates to the left limb, that is, the left arm or leg. In addition, the pain may manifest in the region of the heart, in the back and not only in the region of the spine, but, for example, in the ribs, and so on. In this case, it is particularly important to pay attention to the nature of the change in pain depending on the patient’s actions, comparing the feelings of back pain with, for example, leg pain. If the patient is sitting for a long time and has pain or numbness in his leg, a discomfort in the lower back, and after a little warm-up or walking the pain is gone, this will be an indirect sign that determines lumbar osteochondrosis of the spine. It can be the same image with the neck and arms. In summary, the main symptoms of osteochondrosis include back pain and discomfort. In the event that these symptoms coincide with pain in other parts of the body, osteochondrosis may become more complicated with protrusion, disc herniation, and a compressed nerve.
In addition, I would like to draw attention to the fact that even with the onset of the first pain in the spine, special attention should be paid to this malaise. After all, osteochondrosis may not manifest itself weakly or for a long time at all. However, it continues to develop successfully in the spine, leading to the degradation of more and more plates. Therefore, a simultaneous visit to the doctor allows for an earlier diagnosis of osteochondrosis, which facilitates its treatment.
Osteochondrosis and salt deposition
Osteophytes or hook-like growths of the vertebrae appear to reduce the load on the intervertebral discs. In this case, the appearance of osteophytes impairs the mobility of the intervertebral joints.
The common belief in everyday life that salt deposition is the main cause of osteochondrosis is wrong. Therefore, treating osteochondrosis with a salt-free diet is meaningless.
The most common complaints of osteochondrosis of the spine
The most common complaints of osteochondrosis are:
- Discomfort in different parts of the spine. The pain can be minor, dull, pulling and strong, sometimes very intense and unbearable - with lumbago.
- Increased fatigue in the workplace, both physical and mental.
- Sensory damage to the limbs and different parts of the body, coldness in the arms or legs.
- Pain radiating to the legs, nerve trunks.
- Pain radiating to the shoulder blades, shoulders, and pain in the neck and headrests.
- Cervical osteochondrosis is often accompanied by headache, dizziness. Increased visual fatigue or decreased visual acuity are often observed.
- With overcoming the lumbar-sacral region, disorders of the reproductive system are common - various sexual dysfunctions. Therefore, in most men, sexual strength increases after treatment. In women, the normal functioning of the lumbosacral zone increases the likelihood of conception and contributes to a comfortable pregnancy.
Diagnosis of osteochondrosis
A history should be collected to diagnose osteochondrosis. In this case, it is essential to establish the patient’s complaints. Certain symptoms of osteochondrosis are quite typical. Others, on the other hand, need to be distinguished from signs of other diseases. It is important that neural, vascular, trophic disorders in osteochondrosis can simulate various diseases, such as angina pectoris, gastritis, gastric ulcer, acute surgical diseases of the abdominal organs. Therefore, all symptoms should be carefully analyzed to avoid misdiagnosis and subsequent prescribing of incorrect treatment.
When collecting a medical history, including patient complaints, current medical history, and patient life, the physician monitors his or her age because osteochondrosis develops more often in older people and from the onset of symptoms to the time the patient disappears to the physician. In osteochondrosis, slow development is characterized by periods of exacerbation periodically replaced by periods of remission. Additional research methods are prescribed to clarify the diagnosis.
X-rays for osteochondrosis
The most available method for diagnosing osteochondrosis is, however, X-ray examination is quite informative. There are several X-ray methods for diagnosing the disease:
Smooth X-ray of the spine is the simplest X-ray method to diagnose osteochondrosis. Its essence is the X-ray of the whole or individual segments of the spine. Most often, vision radiography is performed - the location of the spinal lesion is determined based on the symptoms of the disease and the patient’s complaints. X-rays of the spinal segment affected by osteochondrosis show a decrease in the thickness (atrophy) of the intervertebral plates, which is manifested in a decrease in the space between the vertebrae, in the appearance of the bone. outgrowths of the vertebral bodies - osteophytes, partial dissolution - absorption of bone tissue from the vertebral body, changes in the shape of the spinal segment, such as smoothing of lumbar lordosis.
Myelography is a more complex and dangerous diagnostic method. In such a test, a certain amount of contrast fluid is injected into the spinal canal. The risk of this test method is the possibility of allergic reactions to the contrast agent or the risk of spinal cord damage during spinal puncture. Myelography can be used to determine the internal structure of the spinal canal. This method is particularly informative for the definition of spinal hernias.
Computed tomography and magnetic resonance imaging are the most modern, yet the most expensive and hardest to access method for diagnosing osteochondrosis. These diagnostic methods are commonly used to distinguish between osteochondrosis and other diseases of the spine that have similar symptoms, such as spinal cancers.
A neurological examination of a patient with osteochondrosis is mandatory for a comprehensive assessment of the patient's condition. Neurological consultation can clarify the localization and extent of motor and sensory disorders.
Treatment of osteochondrosis
The clinic provides effective treatment for all forms of osteochondrosis. Treatment is performed on an outpatient basis. The treatment is based on a comprehensive program aimed at the rapid elimination of the underlying syndrome and the cause of the suffering. The following methods can be used as part of complex therapy:
- acupuncture;
- vacuum therapy;
- gentle manual therapy techniques (post-isometric relaxation);
- laser therapy;
- pharmacopuncture;
- dry adhesion;
- magnetopuncture;
- electrical stimulation and other treatment methods.
The treatment process averages 10-15 sessions, and the elimination of acute pain syndrome is 1-3 sessions.
The earlier the treatment starts, the better the result will be!
Is complete elimination of osteochondrosis real?
It depends on the form of the disease, the severity, correctness and timeliness of the treatment. Complete recovery is only possible in the initial stage.
But exacerbations of osteochondrosis can be prevented by not feeling pain for years. If a person has suffered from osteochondrosis but does not feel discomfort now, it does not mean that it has passed without a trace. There may be changes in the spine.
The main task is to stop the development of the disease and to do everything possible to ensure that some of the abnormalities of the spine disappear, the symptoms disappear or decrease (back pain, cold slenderness and numbness of the arms, legs, headache, etc. ). ).



































